Returning to Competitive Play After COVID Infection, When Is It Safe?
While Long COVID is an established source of chronic disability months after COVID infection, active people, particularly young competitive athletes, may have a more ominous risk after COVID. Although COVID affects competitive athletes at similar rates compared to the general population, the cardiovascular implications, and their ability to resume athletic participation remain unclear. Of particular concern is viral myocarditis which is cardiovascular inflammation that is associated with a significant portion of sudden cardiac death (SCD) in athletes (ranging from 5 to 22% pre-COVID). The severity of COVID-associated myocarditis may reflect the immune response generated by the host, so young healthy athletes may generate a more robust immunologic reaction to viral infection and experience greater bodily harm. A viral prodrome (sinus congestion, runny nose, cough, and fever) may precede viral myocarditis. Young patients, particularly athletes may present with severe chest pain with electrocardiogram (ECG) abnormalities, various degrees of exertional shortness of breath, palpitations, and generalized fatigue. In extreme cases, people may present with decompensated congestive heart failure. The most catastrophic presentation of viral myocarditis is a life-threatening arrhythmia or sudden cardiac death resulting from heart damage.
Fortunately, the prevalence of myocarditis in COVID-19 is now thought to be extremely rare as large retrospective multi-center cohort studies have found it to be 1% or less. Nonetheless, when new symptoms after COVID such as chest pain or palpitations raise concern for myocarditis, an expert panel from the American College of Cardiology/American Heart Association (ACC/AHA) recommends a selective cardiac evaluation, especially for athletes wanting to return to competitive play. Exercising with active myocarditis can lead to increased inflammation and a proarrhythmic environment. Furthermore, even in the absence of COVID, since intense exercise can lead to transient elevations in blood cardiac enzyme levels and imaging findings suggestive of cardiac fatigue and myocardial inflammation, the athletic heart can have abnormalities difficult to distinguish from the COVID inflamed or injured heart.
So, when may an athlete safely return to play (RTP) after a COVID infection? If COVID viral myocarditis is suspected by the provider based on symptoms, current ACC/AHA guidelines recommend a 10 day rest period after symptom resolution. In addition, the provider should obtain SARS-CoV-2 polymerase chain reaction (PCR) testing or antibodies, biomarkers of myocardial injury with blood troponin levels, and the serum inflammatory marker, C-reactive protein. Finally, a cardiac evaluation with an ECG and cardiac ultrasound (echocardiogram) is necessary. Nonetheless, given the nonspecific nature of biomarkers, symptoms, ECG, and echocardiogram findings in myocarditis, cardiac magnetic resonance imaging (CMR) may be needed as the noninvasive gold standard to evaluate myocardial inflammation, including segments not ideal for biopsy. On CMR, there are three diagnostic criteria for viral myocarditis – swelling, bleeding, and cell death.
Several cardiology societies have made recommendations for RTP post COVID for athletes (see table below), but I will highlight the ACC/AHA guidelines. According to the AHA/ACC, adult athletes should abstain from exercise for 10 days following an asymptomatic diagnosis or symptom resolution from COVID and gradually return to their previous level of activity with athletic trainer supervision. Meanwhile, mildly symptomatic athletes recovering from COVID do not require extensive risk stratification beyond history and physical exams if their mild symptoms are self-limiting. However, in athletes with moderate to severe or not self-resolving symptoms, cardiovascular testing is needed, including ECG, cardiac biomarkers, and an echocardiogram. If testing is normal, then athletes may RTP gradually with the supervision of athletic trainers. But abnormal testing warrants a CMR to confirm the diagnosis, and ACC/AHA myocarditis guidelines recommend abstaining from competitive play for 3-6 months for those athletes with a confirmed diagnosis.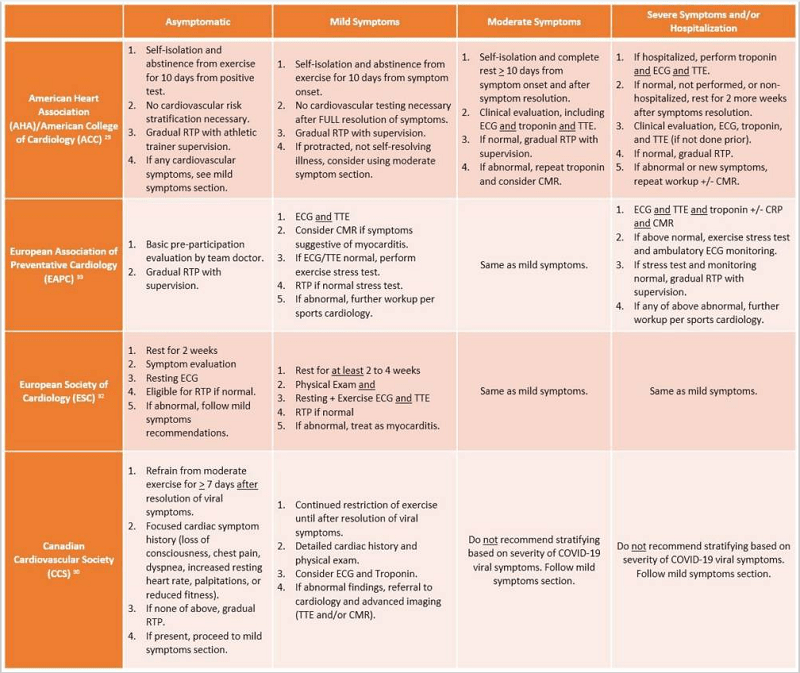
References:
- Summary of return to play (RTP) recommendations from major cardiology societies. ECG, electrocardiogram; TTE, transthoracic echocardiogram; CMR, cardiac magnetic resonance imaging; CRP, C-reactive protein. (Khan, 2021)
- Chilazi, M , COVID, and Cardiovascular Disease: What We Know in 2021, Current Atherosclerosis Reports (2021) 23:37
- Roth, A DO Addressing the Long COVID Crisis: Integrative Health and Long COVID
- Global Advances in Health and Medicine Volume 10: 1–6, October 13, 2021
- Khan, Z Review of COVID-19 Myocarditis in Competitive Athletes: Legitimate Concern or Fake News? Frontiers in Cardiovascular Medicine | www.frontiersin.org 1 July 2021 | Volume 8
