Pulmonary Emboli
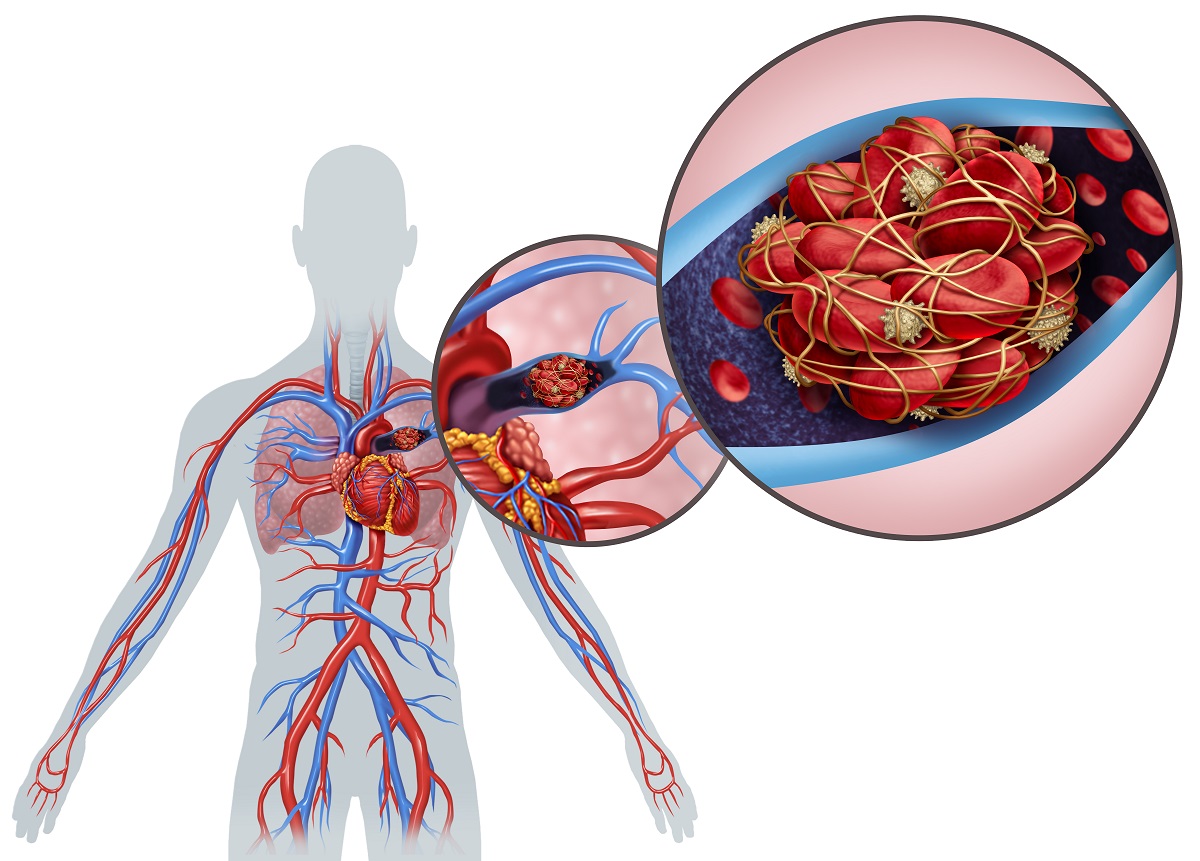
Pulmonary emboli (PE) are blood clots that occur in the arteries that carry blood from the right side of the heart to the lungs. Most often, these clots are formed in the deep veins of the legs and migrate to the heart and subsequently to the pulmonary vasculature.
If pulmonary emboli are large and occlude a significant part of the vessels in the lungs, they can have dire consequences and be life-threatening. With a large pulmonary embolism, blood flow to the lungs is blocked, and therefore blood cannot exchange oxygen nor deliver that oxygenated blood to the rest of the body.
Furthermore, a large clot serves as a clog in the cardiac circuit such that the pressure in the right side of the heart acutely increases as it tries to push blood past the clot. This can result in acute right-sided heart failure. However, if caught early, there are many available treatments, and patients can fully recover. If you suspect you may have a PE, please seek medical attention immediately.
You May Be at Increased Risk of a PE If You Have:
- Underlying conditions that cause inflammation, such as active cancer, recent surgeries, or COVID-19;
- Cardiac disease, particularly heart failure;
- Hereditary blood clotting disorders;
- Vascular trauma;
- Smoking;
- Obesity;
- Pregnancy;
- Supplemental estrogen therapy in the form of birth control or hormone replacement therapy;
- Prolonged immobility – bed rest, recent surgery, etc.;
- Long trips by plane, car or train with little walking.
What Are The Symptoms of a PE?
- Shortness of breath;
- Cough, potentially coughing up blood;
- Chest pain or pressure, usually sharp in quality;
- Chest pain that is worse with a deep breath;
- Leg swelling, readiness, or pain; usually only one leg;
- Lightheadedness;
- Fever.
How Is a PE Diagnosed?
When there is clinical suspicion of a PE, your doctor will often run a number of tests. A blood test called a D-dimer can be used to check your blood for a protein fragment that is present in high concentrations when your body is forming or breaking down a blood clot. If this test is negative it rules out a PE or DVT. If it is positive, it does not necessarily mean you have a PE or DVT. The D-dimer test can be positive when no clot is present if other risk factors for inflammation are present, for example, recent surgery, cancer or smoking. In this case, further imaging testing is done.
Imaging tests include a CT scan with contrast dye that can highlight the blood clot in your lungs. If you are not able to get contrast dye either because of an allergy to it or because of kidney dysfunction, then another imaging test called a ventilation-perfusion scan (aka VQ scan) is often performed. A VQ scan is a study that compares airflow and blood flow in the lungs. In normal lungs, all lung tissue gets both air flow and blood flow. However, in the setting of a PE, all lung tissue will still get airflow, but the PE will block blood flow to part of the lung tissue, so there will be a mismatch between ventilation (i.e., airflow) and perfusion (i.e., blood flow). Your doctor may also order an ultrasound of the veins in your legs to investigate whether a clot is present there to explain why you may have a PE.

A number of tests are also done to see if your heart is under strain from the PE. These include blood tests called a BNP level and a troponin level. An echocardiogram, or ultrasound of your heart, is also often performed to assess your cardiac function, particularly of the right side of your heart. The results of these tests can help determine what treatment strategy is best for you.
What Is The Treatment for a PE?
The main goal of treatment for a PE is to dissolve the clot in the lung to restore blood flow to the lungs and relieve pressure on the right side of the heart. In most cases, this is done by starting blood thinners that prevent the clot from getting bigger and allow your body to dissolve the clot. In severe cases when a PE is acutely life-threatening, we do not have time to wait for the blood thinners to dissolve the clot, which happens over the course of weeks to months. In these cases, higher potency blood thinners are used in a process called thrombolysis. In some cases, the extent of the clot is so great that a surgical procedure is needed to remove the clot. This is called a surgical embolectomy.
Regardless of the means of treatment at the time of diagnosis, patients generally remain on blood thinners for a number of months, and sometimes indefinitely, after diagnosis to prevent recurrence of the clot. In patients who cannot tolerate blood thinners due to increased bleeding risk, sometimes an IVC filter is placed in the leg to prevent clots that may form there from migrating to the lung.
LOCATIONS
Contact us for more information.