Diastolic heart failure: a failure to relax
What is diastolic heart failure?
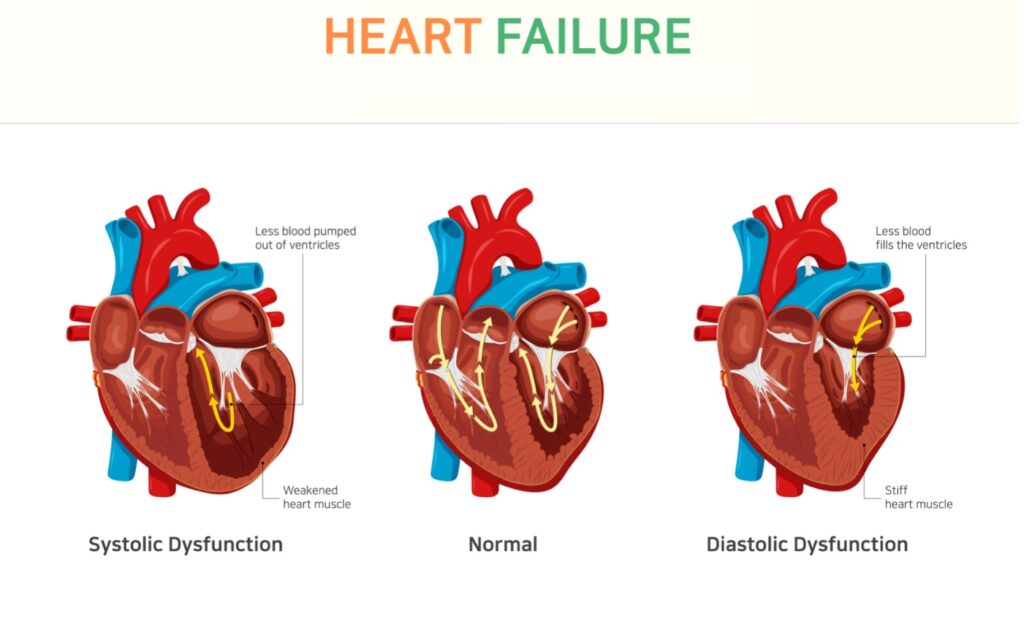
In gross terms, ‘heart failure’ refers to the inability of the heart to properly do the job of pumping oxygen-rich blood to the body. But ‘heart failure’ is not confined to the inability of the heart to contract, called systolic dysfunction. The more common type of heart failure occurs when the heart stiffens and is unable to properly fill with blood during the relaxation phase of the cardiac cycle. Therefore, with each cardiac contraction, an inadequate amount of blood is circulated to the body. In order to try to overcome this stiffness, the heart increases the pressure with which it fills with blood in an effort to increase the blood volume. This in turn increases the pressures in the lungs and the venous system that is returning blood to the heart.
What are the common signs and symptoms of diastolic heart failure?
The result is the classic signs and symptoms of heart failure including shortness of breath with exertion or when lying down, swelling in the ankles, legs or abdomen, and exertional fatigue.
What causes diastolic heart failure?
We will all get some degree of diastolic dysfunction as we age. Stiffening of the heart muscle is a natural consequence of getting older. However, there are also a number of factors that accelerate the process of cardiac stiffening and can contribute to premature and more severe diastolic heart failure. These include the following:
- High blood pressure (Hypertension)
- High cholesterol (Hyperlipidemia)
- Obesity
- Coronary artery disease
- Diabetes
- Valvular heart disease
- Pericardial disease
- Sleep apnea
How is diastolic heart failure diagnosed?
A cardiologists’ suspicion that a patient has diastolic dysfunction is raised during an appointment when the patient and the doctor discuss the patient’s medical history and symptoms they may be having. The physical exam can also show signs of heart failure.
An echocardiogram, a non-invasive ultrasound imaging test, is an invaluable tool in diagnosing diastolic heart failure. Your cardiologist is able to use the echocardiogram to look at the structure and function of your heart and assess the pressures in the heart. In some cases, a more invasive test referred to as a right heart catheterization is needed to better assess cardiac pressures and heart function.
How is diastolic heart failure treated?
Treating diastolic heart failure is difficult. Many of the treatments that have been developed and validated for systolic heart failure have not been shown to have significant mortality benefit in diastolic dysfunction. However, some treatments can have clinical benefit in relieving symptoms of diastolic heart failure. These include medications such as diuretics which help reduce blood volume and medications that lower your heart rate and prevent arrhythmias such as atrial fibrillation. It is also very important to treat the risk factors for diastolic dysfunction as mentioned above to prevent the onset or worsening of the condition.
For any questions concerning your heart health and diastolic heart failure diagnosis and treatment, please, contact us and we will schedule a cardiovascular risk assessment to evaluate possible risks of a heart disease.
